Some health workers at Health NZ public hospitals and services are planning to strike on Thursday 23 October to 7am on Friday 24 October. Emergency departments will be open for emergencies only. Strikes planned for 23 to 24 October 2025external link
Obstructive sleep apnoea Mate hoto hau
Normally when you go to sleep your throat muscles hold your airway open. But if you have obstructive sleep apnoea, your throat muscles relax too much when you are asleep. This causes pauses in your breathing. These breathing pauses can lead to disrupted sleep and reduced oxygen levels.
Causes of obstructive sleep apnoea
When you go to sleep, most of the muscles in your body become relaxed and soften. This helps you have a comfortable and relaxed sleep. The muscles of the roof of your mouth (the soft palate) and tongue remain firm and toned enough to allow clear passage of air through the throat and in and out of the lungs.
This lets you get quality sleep without any breathing problems.
Snoring
Snoring is a noise made by vibration of the soft palate and other soft tissue due to narrowing in the throat while breathing when asleep. This happens because the muscles controlling the soft palate and tongue relax too much and narrow the airway to the lungs. The breathing muscles then have to work much harder than normal to get air into the lungs.
Snoring is not generally considered a health risk, but because sleep during snoring is not as relaxed and comfortable, you may feel less refreshed in the morning and more tired during the day. Snoring can also affect your social life and relationships.
Snoring results from a narrowing of the throat. In some people, their muscles relax so much that the airway becomes completely blocked, causing the airflow to stop. This is called apnoea, meaning 'lack of breath'.
Apnoea
Apnoea can last 10 seconds or more, and can be repeated hundreds of times a night.
During the apnoea, you automatically make an effort to breathe against the blocked airway. The brain soon recognises there is a problem and leads you to a lighter level of sleep or wakes you up.
This allows the muscles to firm up, which in turn opens the airway to allow breathing to begin again.
As you relax back into sleep, the cycle of snoring and apnoea can repeat itself, and do so many times during the night. This repeated disruption to sleep often causes you to feel sleepy during the daytime.
Who can get obstructive sleep apnoea
While obstructive sleep apnoea can affect anybody, it is more common in:
- middle-aged people — especially men
- people who are overweight, especially round the face, neck and middle
- people who snore.
Symptoms of obstructive sleep apnoea
Symptoms of obstructive sleep apnoea include:
- snoring
- stopping breathing during sleep
- being sleepy during the daytime
- waking with a headache
- poor memory or concentration
- getting up to the toilet several times a night
- high blood pressure
- sexual dysfunction
- irritability, mood changes or depression.
If untreated, obstructive sleep apnoea can cause:
- work accidents if you have a high-risk occupation, for example, if you are a heavy machine operator
- motor vehicle accidents
- short-term memory problems
- depression
- high blood pressure (hypertension)
- irregular heartbeat (arrhythmia)
- cardiovascular diseases such as heart disease and stroke.
Diagnosing obstructive sleep apnoea
Your healthcare provider will ask you questions about your symptoms and examine you.
They may also ask you to complete a questionnaire called the Epworth sleepiness scale.
Epworth sleepiness scale — Harvard Medical Schoolexternal link
If they are concerned about obstructive sleep apnoea, they will arrange for you to have a sleep assessment.
Sleep assessment
If your healthcare provider thinks you have obstructive sleep apnoea or another sleep disorder, they may recommend that you have a sleep assessment.
- Some healthcare providers are trained to provide sleep assessments. If your healthcare provider is not an approved provider, they can refer you to someone else in the community.
- Sometimes you may need a more complex type of assessment, which needs to be done at a hospital or sleep clinic.
- You may prefer to pay to see a private sleep clinic.
A simple sleep assessment takes around half an hour. You may be able to get your assessment funded or subsidised by Health New Zealand.
A sleep assessment involves several tests, including:
- measuring your body mass index and neck circumference
- checking your blood pressure
- examining your mouth and nose
- testing to see how well you can breathe through your nose
- checking for related health problems, such as heart or lung disease.
The person doing the assessment will ask you questions about:
- your sleep
- your lifestyle and daily routine
- what you normally eat and drink
- your whānau
- your family history
- what medications you take.
This is to give the assessor a better idea of what might be affecting your sleep and how badly your sleep is affecting your lifestyle.
They may ask you to complete 2 questionnaires.
The Berlin questionnaire is used to assess your risk of having obstructive sleep apnoea.
Berlin questionnaire — National Sleep Diagnosticsexternal link
The Epworth sleepiness scale questionnaire is used to assess your daytime sleepiness.
Epworth sleepiness scale — Harvard Medical Schoolexternal link
The questionnaire results will be filed with your sleep assessment documentation and looked at by your hospital's sleep health services when they review your sleep assessment report.
You may be asked to undergo an overnight oximetry test. You will be given an oximeter to take home and wear while you sleep. On the night of the study, you will need to keep a sleep diary (this also includes instructions for using the oximeter). Return the oximeter and diary to the assessor the next day. The results will be included in the sleep assessment report.
If you do not have obstructive sleep apnoea, you may need to see your healthcare provider to check for other problems or for advice to manage your symptoms.
If you have obstructive sleep apnoea and you meet treatment criteria, you may be offered treatment through a sleep health service (sleep lab).
If you have obstructive sleep apnoea but do not meet the treatment criteria, your healthcare provider will manage your care and treatment.
If your diagnosis is uncertain, you may need more tests.
Treating obstructive sleep apnoea
If you are overweight, try to lose weight. Losing weight, even 5 to 10% of your body weight, may help improve your symptoms as well as help other health problems, such as:
- high blood pressure
- diabetes
- high cholesterol
- joint problems.
You should also:
- quit smoking if you smoke
- avoid alcohol and medicines that make you sleepy before bed
- be physically active — aim to do at least 30 minutes of moderate activity most days
- maintain good sleep habits
- sleep on your side and avoid sleeping on your back. If side sleeping is not your natural sleeping position try using pillows in one or more places on your bed that help keep you from rolling onto your back.
As well as self care measures, if you have severe obstructive sleep apnoea, other medical issues or drive or operate machinery or aircraft for a living, you will need medical treatment.
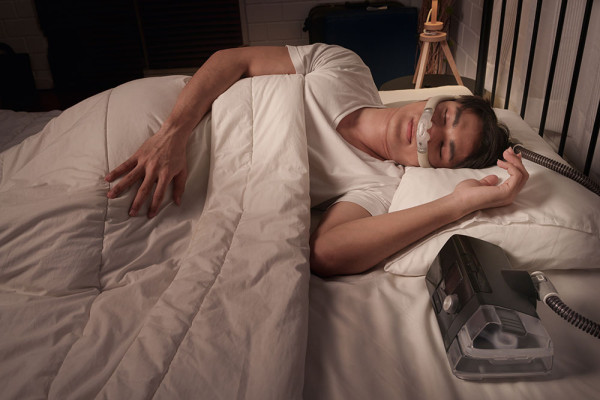
Continuous positive airway pressure (CPAP) therapy
CPAP is a device that treats obstructive sleep apnoea. It blows air through your nose (or nose and mouth) into your throat. The airflow supports your throat muscles and keeps your airway open. This prevents the pauses in your breathing and helps you sleep better. Sleeping better stops you feeling as tired throughout the day and improves your overall health.
You need to wear a well-fitted mask connected to the device by a tube when you are sleeping.
The device is very quiet. Some people also use a humidifier to make the air less dry.
CPAP starts working straight away and also stops snoring.
It is important to use the machine every night. This includes taking it with you if you are sleeping away from home.
You may qualify for publicly funded CPAP therapy. If you do, you will be offered a CPAP trial through a sleep health service. If you do not meet the criteria, you may wish to seek CPAP therapy through a private provider.
If you are on a benefit or low income, Work and Income may help you pay for CPAP therapy. Talk to your usual healthcare provider or sleep assessment provider for more details.
Oral appliances
These are also called mandibular advancement splints. They are devices that you put in your mouth when you go to bed.
Oral appliances work by pushing your jaw forward, which opens up your airways to help you breathe and reduce snoring.
You can get oral appliances from:
- pharmacies and online stores, which you fit yourself
- a sleep specialist, who will refer you to a hospital dental service for a custom-fitted appliance. Your community dentist may also be able to provide this.
Surgery
Some people with breathing problems in their sleep may need surgery on their upper airways. Or they might need other surgical treatments, such as tonsillectomy, which can be helpful for adults with large tonsils, or nasal surgery.
Your healthcare provider, such as your doctor or sleep specialist, can refer you for surgery if you meet the criteria.